When AI Misdiagnoses: Who Pays the Price for Medical Errors? The Age of AI-driven Human Errors!
Table of Content
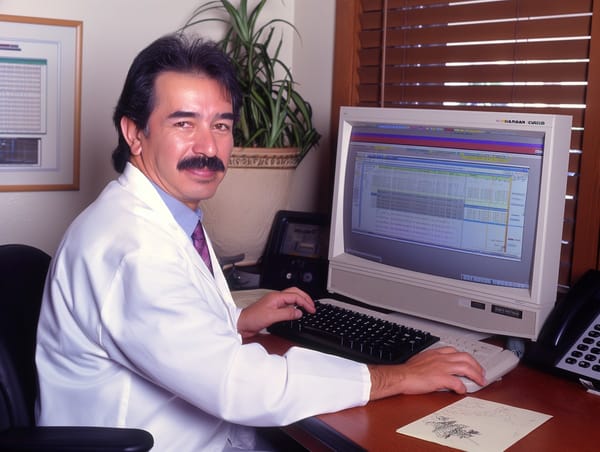
As a doctor and developer, I've spent years on both sides of the table—treating patients and coding software that streamlines healthcare processes. AI is supposed to be the great equalizer, reducing human error and improving diagnostic efficiency.
Yet, here we are in the end of 2024, and I’m more skeptical than ever about AI’s role in healthcare.
Let’s be clear: AI is not your doctor. But too many patients, and even healthcare providers, are starting to think it is.
Self-diagnosing with AI tools has become the norm. Instead of consulting a physician, patients are typing symptoms into AI-powered apps, and often, they’re getting misleading advice. The consequences? Misdiagnoses, delayed treatments, and in the worst cases, serious health complications.
But the problem goes deeper than this. Even in hospitals, where AI is integrated into medical records and diagnostic systems, we’re facing new risks.
Human error hasn’t vanished; it’s just taken a new form—AI-driven error.
AI is Only as Good as Its Training Data
AI thrives on data, but what happens when that data is flawed? Biases in datasets, incomplete medical records, or outdated information can skew AI’s conclusions. AI doesn’t "understand" medicine the way a trained doctor does.
It predicts outcomes based on patterns. If those patterns are faulty, the AI’s diagnosis is too.
Imagine an AI system trained primarily on data from Western hospitals trying to diagnose a patient in a Middle Eastern clinic. The data gap could lead to completely inaccurate conclusions.
And who’s responsible when this happens?
Poor Implementation and RAG (Retrieval-Augmented Generation)
Implementing AI in healthcare isn’t plug-and-play. Get it wrong, and you're opening the floodgates for errors. Retrieval-Augmented Generation (RAG) systems, which combine GPT models with external knowledge bases, can pull in irrelevant or outdated information if the integration is sloppy.
A poorly integrated RAG system might spit out conflicting diagnoses depending on how the prompt is phrased. And let’s be honest: doctors don’t have time to write perfectly structured prompts while dealing with critical cases.
One symptom omitted, one nuance missed—and AI might lead you down the wrong path.
The Problem with Prompts
Every prompt variation could lead to a different AI conclusion.
Prompt engineering isn’t just for tech nerds. In AI-driven healthcare, doctors now have to be part-time prompt engineers. But no physician under pressure wants to stop mid-diagnosis to carefully craft a detailed AI prompt.
Doctors are human. They’re tired, stressed, and sometimes, overworked. Expecting them to interface with AI like a programmer is unrealistic. And every prompt variation could lead to a different AI conclusion.
Imagine the horror of missing a life-threatening diagnosis because the AI wasn’t "prompted" correctly.
Accountability and Ethical Issues
So, who’s accountable when AI gets it wrong?
If a misdiagnosis occurs, is the blame on the doctor, the AI, the developers, or the hospital that approved the system? Accountability in AI-driven healthcare is a legal and ethical minefield. When patients lose trust, the entire healthcare system suffers.
As a developer, I understand the excitement around AI. But as a doctor, I know that misplaced faith in technology can cost lives.
AI Misdiagnosis and a Lesson in Caution
A few days ago, a friend who had recently returned to Asia from London asked if he could perform wet cupping (hijama) on his teenage son, who had jaundice. The mention of liver cirrhosis immediately raised red flags.
Through a series of questions, I discovered the source: an AI-generated diagnosis, backed by his doctor. As an engineer, my friend trusts AI tools, but this was clearly a case where AI had failed.
Diagnosing liver cirrhosis based only on jaundice in a teenager made no sense.
I urged him to get proper testing, suspecting a more common issue like Hepatitis A. The results confirmed it his son have Hepatitis A, not liver cirrhosis.
This was a reminder that while AI can assist, it can also mislead. In healthcare, human judgment is irreplaceable.
Who is responsible for this.
Recommendations for Healthcare Startups
If you're a healthcare startup integrating AI, here are my recommendations to minimize these risks:
- Transparency in Data Sources: Clearly disclose what datasets your AI models are trained on. Avoid hidden biases.
- Human Oversight: AI should assist, not replace. Always ensure there’s a qualified medical professional reviewing AI-driven conclusions.
- Simplify AI Interfaces: Doctors need user-friendly systems, not complex prompt interfaces. Design intuitive workflows that reduce cognitive load.
- Rigorously Test Integrations: Conduct thorough testing when integrating AI with medical records or RAG systems. Edge cases can’t be ignored.
- User Training: Provide hands-on AI training for healthcare staff. They need to understand what AI can’t do, not just what it can.
- Legal and Ethical Safeguards: Implement clear policies around accountability. Know who’s responsible when things go wrong.
- Focus on Automation First: Use AI for automating administrative tasks before jumping to diagnostics. Reduce errors in low-risk areas first.
- Regular Audits: Periodically audit your AI systems for performance, bias, and accuracy.
AI has potential, but healthcare isn’t a playground. If we’re not careful, AI will introduce new forms of human error rather than reducing them. Until we solve these issues, doctors need to stay vigilant, patients need to stay skeptical, and developers—like me—need to remember that lives are on the line.
For more perspectives, check out these detailed articles:
- When AI Misdiagnoses: Can Health IT Be Held Accountable for Malpractice?
- Why Doctors Should Fear AI-Powered Diagnostics
- Can Poorly Designed EMRs Lead to Medical Malpractice? A Doctor’s Perspective on Security and Patient Safety
- How Hospitals Can Automate Tasks
It’s a brave new world, but let’s not be blindly optimistic. AI is a tool—not a savior.